COVID-19’s racial health inequities call for a novel collaborative approach

COVID-19 has become the deadliest pandemic for many, if not all, nations. This has caused healthcare professionals, scientists, health systems, policymakers and others around the world to search for solutions to this global crisis.
Research and innovation must rapidly evolve, and a global collective intelligence needs to emerge to solve COVID-19 and its illumination and amplification of the racial health equity chasm. These crises highlight the need for multiple perspectives to address and curtail their pervasiveness.
Exposing deficiencies
The COVID-19 pandemic led to shortages of personal protective equipment, ventilators and drugs. This level of disruption that goes beyond the walls of healthcare organizations has greatly affected care delivery within their walls. Thus, there is a need to easily assemble thought leaders beyond clinicians and health policy professionals.
Addressing the impact of the COVID-19 pandemic, and others like it, requires platforms that facilitate coordination on two levels: 1) collaboration among entities from multiple sectors and 2) team science, collectively referred to as “integrated coaction.”
Collaboration platforms that (i) connect thought leaders, (ii) share their collective knowledge, (iii) facilitate cooperation among multiple sectors, including life sciences, academia, transportation and distribution, government, and information technology, and (iv) disseminate advancements in immunology and novel medical and scientific breakthroughs are vital.
Agencies such as the National Institutes of Health, the National Academy of Sciences, the National Science Foundation and private organizations have specific initiatives and funding targeting transdisciplinary research and strongly recommend broader collaboration via team science. The collective intelligence of transdisciplinary teams facilitates development of radical innovations in research, address complex medical conditions, and improve human health.1
Additionally, leveraging a flexible, readied catalytic framework designed to improve collaboration across non-scientific and scientific divides and promote shared vision will result in rapid generation of novel solutions to address pandemics. Despite the investment and interest in transdisciplinary research and team science, there are few platforms that facilitate integrated coaction.
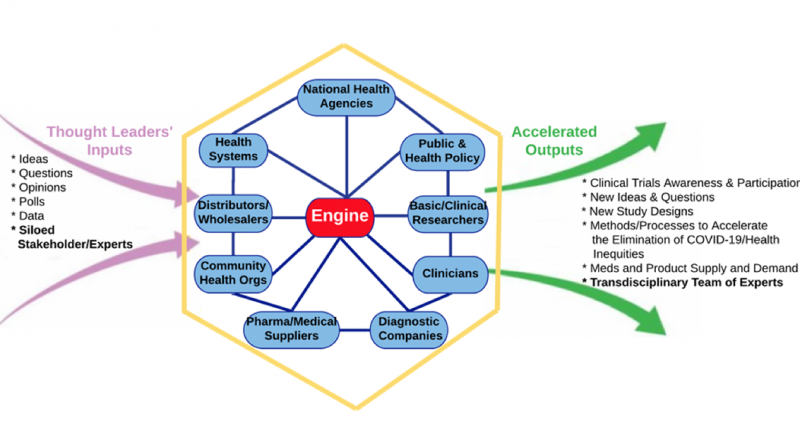
The image above depicts an integrated coaction model, or iCaM, which is ideal for addressing complex multi-specialty parameters associated with health inequities and COVID-19. iCaM is powered by the “engine,” a collaboration platform in this example, that enables the “accelerators,” which are the contributors inside the hexagon, to autonomously contribute information, knowledge, and artifacts or to do so as part of a unified transdisciplinary team.
The structure of iCaM is based on a peer-to-peer network – a dense cluster of people and organizations. This type of structure is purposeful and is built upon the concept of accelerators connecting directly and non-hierarchically to as many accelerators as needed, in a cooperative fashion, to address pandemics and health inequities. The lack of dependency on a single accelerator allows and ensures that each accelerator participates fully in information exchange.2
By way of the P2P network design, iCaM enables accelerators to dynamically self-organize, respond to changing demands and conditions, and convert and translate knowledge contributions into actionable outcomes.
When each accelerator becomes a generative and recipient node in the network dynamic interactions happen because everyone leads and follows, reciprocity and transparency become fundamental values, and continued engagement and success come through collaborative connections2.
Why this approach, and why now?
Health inequities can be traced to the mid-nineteenth century, where researchers recognized that social and class inequalities led to inequities in health.3 Yet, more than 200 years since the origins of health inequities COVID-19 has illuminated their continued existence, especially racial health inequities. SARS-CoV-2 infects and kills African Americans and Latino Americans at a disproportionate and alarming rate.4
This egregious deficiency in our healthcare system demands a different approach – iCaM is just that. iCaM facilitates collaborations around genetic or biological factors predisposing individuals to high risk, impact of social determinants of health on disease development and progression, epidemiology and accurate data collection and sharing, improvements in health systems, clinical trials recruitment, effective treatment, and community-based prevention and mitigation interventions.
COVID-19 adversely impacts the most vulnerable populations, such as older adults and those with hypertension, asthma, cardiovascular disease, and diabetes (all of which are prevalent amongst racial minorities) experience worse outcomes.4,5
Given this health disparity and the complexity of the biochemistry of SARS-CoV-2, the development of creative and productive partnerships (among individuals trained in different fields) powered by innovative technology aimed at addressing COVID-19 and inherent racial health inequities is immeasurably important.
The intellectual integration of transdisciplinary engagement within the trusted environment of the iCaM can facilitate comprehensive understanding and novel and rapid approaches to addressing COVID-19 and associated health disparities in a manner that can lead to scientific breakthroughs.
Now, imagine an accelerator collective, consisting of clinicians, basic and clinical researchers, public and health policy professionals, pharmaceutical and medical product suppliers, national health agencies from around the world, laboratory and diagnostics companies, and distributors. The common union among them being a shared vision and a purpose to contribute, leverage, process, and act upon the various inputs of iCaM.
iCaM provides collaborative capabilities via its engine. The accelerators use the capabilities in an iterative fashion to harness initial knowledge contributions into a collective intelligence that results in policy, community, system and environmental changes that will accelerate health equity, reduce health disparities, and an appropriate response to global health and social pandemics.
Conclusions
Health equity demands different approaches, and COVID-19 has demonstrated that our current and historical approaches are insufficient. As a result, we are at a sentinel moment, especially as it pertains to the need to address health disparities and inequities more effectively.
Thus, novel approaches that can help eliminate the COVID-19 pandemic and address the complex relationships between determinants of health that contribute to health disparities and inequities are in urgent need.
We propose a theoretical, yet practical iCaM, powered by a collaboration platform that provides a mechanism to foster shared intelligence vital to improving health outcomes6. This shared intelligence, derived from champions of transdisciplinary research united on identifying leading strategies and treatment approaches, defines a transdisciplinary approach that galvanizes and realigns our commitment to eliminate inequities.
References:
Horowitz CR, Shameer, K., Gabrilove, J., Atreja, A., Shepard, P., Goytia, C.N., Smith, G.W., Dudley, J., Manning, R., Bickell, N.A. and Galvez, M.P. Accelerators: Sparking innovation and transdisciplinary team science in disparities research. International Journal of Environmental Research and Public Health. 2017;14(3):225-234.
Baker MN. Peer-to-peer leadership: Why the network is the leader. San Francisco: Berrett-Koehler Publishers; 2014.
Fee E, Gonzalez AR. The history of health equity: Concept and vision Diversity and Equality in Health and Care. 2017;14(3):148-152.
Evans, M.K. Covid’s color line — infectious disease, inequity, and racial justice. New England Journal of Medicine. 2020; 383:408-410.
Paules CI, H.D. M, Fauci AS. Coronavirus infections – more than just the common cold. Journal of the American Medical Association. 2020;323:207-208.
Mirel B, Luo A, Harris M. Research infrastructure for collaborative team science: Challenges in technology-supported workflows in and across laboratories, institutions, and geographies. Seminars in nephrology. Vol 35: Elsevier; 2015:291-302.
Dr. Walter Rayford, is a surgical urologist at University of Tennessee Health Science Center.
This post was coauthored with Randy V Bradley, associate professor of supply chain and information systems management at University of Tennessee’s Haslam College of Business