COVID-19: a technologist’s tale | Healthcare IT News

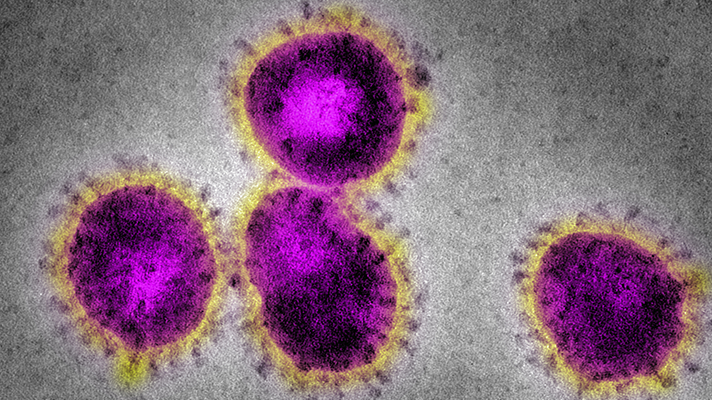
COVID-19 has been deadly, it’s infective and has posed the biggest public health risk to society in almost a hundred years. It’s far from over and whilst the first wave may have occurred there are likely to be subsequent waves which may arrive in the winter months if not sooner. So far we have seen responses from across government, the NHS, local authorities and wider society coupled with industry providing support and in many cases much needed PPE. There has been a lot of attention on tragic deaths, especially in deprived communities.
Amongst these tragic circumstances there has also been a lot of attention on technology in healthcare and public health. Some of that technology is an acceleration of what was already there, some of that technology may be transformative but there has been appetite for change and focus on doing things using technology.
I need some drugs
Analogies are often drawn between the logistics in retail and those in pharmacy. Early on there were many ideas about greater use of online pharmacies, such as Pharmacy2U or Echo. This is only natural as it reduces footfall to physical places and helps avoid the need for those who are most vulnerable in having to leave their homes. Many of the online pharmacies had rapid uptake and a bit like the retailers also had to scale up their workforce to cope with demand. The suppliers to pharmacies were also challenged with ensuring the flow of stock could get to the right places given that much of it is on physical pharmacies.
The other aspect of medication that COVID-19 soon outed was prescribing. What became quite apparent is the lack of digital prescribing in large parts of the NHS. Whilst the system used by NHS General Practice is fairly well embedded, there is nothing similar for private practices or for any hospitals or dental services. This is a gap and adds to the friction for clinicians and their patients. It’s something that digital leaders need to try and solve fairly soon in preparation for any second wave.
The doctor will see you now
Staying at home has meant that many people were driven to use remote services. It seems to have become part of everyone’s lives including the way in which we interact with doctors and other healthcare professionals. During this period we have seen lots of great initiatives to digitise the consultation process, this isn’t anything new but it’s certainly been accelerated with the NHS in England reporting record levels of online consultation. There were already hundreds of video-consultation platforms on the market in England but the COVID-19 period has seen adoption that, dare I say it, is ‘unprecedented’. However, this rapid uptake, adoption and utilisation comes with some hidden challenges and it’s how we deal with those needs that remains hidden. All those people that either can’t use an online platform or won’t use an online platform. There is a real risk of developing inequity in access to health services and we need to address this fairly rapidly so that citizens don’t suffer in the next few months.
The hospital sector has been interesting as it has also had to adopt telehealth at an alarming rate, perhaps not with the same agility as primary care, but adoption has taken place. Although there have been concerns as NHS England and NHSX have in some cases procured national solutions for some hospitals in England, but some may argue those solutions have not been stable and whilst the decision may have been made quickly, failing technology may have generated more work for clinicians and left patients disadvantaged.
You seem a bit hot today
Some sustainability and transformation partnerships and clinical commissioning groups across England have been creative and used the window of opportunity to use telemedicine to their advantage. There will be many examples from across the country, but services such as Doctaly and Medopad are providing much needed remote monitoring services. Whilst the UK has made slow traction previously, COVID-19 has demonstrated that we can quickly catch up. These remote services are helping COVID-19 response teams to monitor patients remotely and identify those that need the most support and help. These telemedicine services seem vital to the ongoing COVID-19 response and certainly something that will probably need to be expanded in preparation for a second wave.
Apps, apps and more apps
The NHS has a troubled history with apps with local and national teams often competing to build in-house products, and thereby competing with industry. You may think that the coronavirus would have eroded some of that competition and opened the doors of collaboration. Unfortunately, the NHS in England hasn’t really managed to offer confidence to citizens with mixed views about designing and deploying tracing applications. There has been much debate about the right approach and the general media reporting internal concerns from within NHSX about credibility. The NHS still has time to get its strategy right on apps but it’s going to need to gain trust and confidence from the population. There is a lot we can learn from other countries around the world and whilst we may chose our own approach in the UK, we probably shouldn’t dismiss what has worked elsewhere.
Queueing, a favourite past time
Hospitals have had to deal with a different patient mix during the pandemic. Much of the traditional work of outpatient referrals, theatre lists and emergency care has been replaced with all things COVID-19. However much of that need still exists in the population, it’s probably queuing up and the risk is that when the next wave arrives so will the unmet need from the population. Those with COVID-19 and those without COVID-19 could be more likely to come into contact if the health system is trying to deal with both sets of needs. North-West London Hospitals have demonstrated that the system can prepare for this by using digital tools designed around local referrers to help deal with these flows, including advice and guidance services. There are many products out there but the Rego product they are using is already helping GPs with seeking advice and managing referrals, which will undoubtedly help with the next wave.
What next?
There is a lot we can learn from the health system response to the first wave and much we can take from colleagues around the world. However, digital leaders at all levels in the system need to act now ahead of winter and before the next wave arrives, using the best of technology to make a difference to peoples lives.